Listen on: Apple Podcasts | Spotify
Natural health practitioners have been warning people about antibiotic use for decades now. Not surprisingly, most of their concerns have fallen on deaf ears.
Today, antibiotic resistance as a public health threat is undeniable.
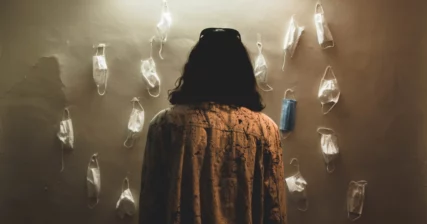
Unfortunately, the COVID pandemic has made that threat even worse, not because of COVID, nor because of an increase in bacterial infections, but because most COVID-positive patients received antibiotic treatments as part of their care. Doctors prescribed them without any evidence they helped patients, but with clear evidence that their prescriptions increased the risk of antibiotic resistance.
A recent paper in the British Medical Journal, titled Delayed antibiotic prescribing to reduce antibiotic use: an urgent care practice change emphasizes the need for medical professionals to limit antibiotic use, pointing out that 45.7% of antibiotic prescriptions are prescribed unnecessarily.
Because so many doctors are already overwhelmed with patient loads, it’s likely many doctors will miss this kind of information. And even if they learn about antibiotic resistance, they may be so steeped in the habit of prescribing antibiotics that they might not change their ways.
This is why it’s crucial for patients and consumers to remain informed, and push back on their doctor’s knee-jerk reactions to antibiotic prescriptions.
Antibiotic Resistance
Without question, antibiotics have saved countless numbers of lives since their introduction to modern medicine in the 1940s. Since then, scientists developed numerous new antibiotic medications in addition to the original: penicillin.
Experts have expressed caution about antibiotic overuse since the mid-1940s, worrying that it may cause antibiotic resistance, the development of bacteria strains immune to the effects of those antibiotics.
Like vaccines that cause the creation of new viral strains (the COVID-19 vaccines being a perfect example), antibiotic drugs cause the creation of new bacterial strains.
New antibiotic-resistant strains of the bacteria that cause pneumonia, tuberculosis, gonorrhea, and salmonellosis make treatment more difficult, take longer, and end up costing more.
Antibiotics in Agriculture
Antibiotic-resistant bacteria don’t come just from humans using antibiotics. Agriculture plays a major role.
To keep animals healthy, especially when they’re kept in close quarters, the animals are routinely given antibiotics. Not surprisingly, the agricultural industry also sees a critical need for alternatives to current antibiotic drugs.
Interestingly, the majority of research on the antibacterial effects of essential oils is done on animals. If farmers can provide a natural alternative to pharmaceuticals, it may slow the development of drug-resistant bacteria. In addition, thousands of plants show antibacterial effects, which could dramatically increase the variety of antibacterial options for farms and ranches.
Antibiotics in Medicine
That’s not to say that the medical community is innocent. Doctors consistently overprescribe antibiotics to patients.
For example, people average two to five colds per year. If they see a doctor for a cold, they usually get an antibiotic prescription, even though the vast majority of colds are caused by viruses, not bacteria, making an antibiotic totally unnecessary and useless.
Most consumers wouldn’t know that, though. They gladly fill and take their prescriptions, trusting that their doctor knows best.
During the first several months of 2020, antibiotic use waned, but that was primarily because people stayed at home, avoided other people, and stayed out of hospitals and clinics except for emergencies of COVID infections.
Interestingly, as more patients visited healthcare facilities for COVID-19, antibiotic prescription rates increased significantly.
As explained in a report by the Office of Science & Data Policy:
A meta-analysis showed that approximately 75% of COVID-19 patients worldwide received antimicrobial drugs, despite estimated rates of bacterial co-infection of 8.6%.
The report goes on to say:
Outbreaks of drug-resistant bacteria and fungi have occurred in facilities treating COVID-19 patients, which may be linked to inappropriate antimicrobial prescribing.
In the United States alone, antibiotic resistance leads to more than 3 million infections and 35,000 deaths annually, a number expected to significantly increase each year if antibiotic use continues at current rates.
In 2019, antibiotic-resistant bacteria killed 1.27 million people globally.

Feel Better Fast. Guaranteed.
Energy+, EDGE, and MentaBiotics make up the Happy Juice supplement stack, with ingredients clinically proven to:
- decrease anxiousness scores by 55%
- decrease irritability scores by 60%
- decrease fatigue by 64%
- decrease anger 54%
- decrease tension by 45%
- decrease confusion by 43%
- decrease overall distress by 49%
- increase good bacteria by 70%
- decrease negative mood by 105%
- increase positive mood by 211%
Other Antibiotic Problems
Antibiotic resistance isn’t the only health problem connected to antibiotic use.
Antibiotics also:
- Weaken the immune system by obliterating the microbiome
- Can lead to mental health problems, especially in children, by wiping good bacteria that produce neurotransmitters like serotonin
- Increase the risk of other infections
- Can cause abdominal pain, nausea, restlessness, and difficulty sleeping
- In rare cases may cause black hairy tongue (look that one up if you want to feel your stomach turn)
Read also: Antibiotics: Are the risks worth the reward?
What should consumers or patients do?
Taking an antibiotic yourself might quickly cure an infection, so on a personal level, you might think that it makes sense. After all, what effect might one patient have?
That’s kind of the same argument you might have to not vote. But what if a new bacterial strain got triggered by your personal use of the antibiotic, just like your one vote could tip the balance in your candidate’s favor?
In addition, the mental health and immune function issues related to antibiotic use are serious, too.
Does that mean everyone should avoid them? No. But we’ve become too accustomed to treating illness with conventional medicine instead of making our bodies overcome the illness with their own immune systems.
The best course of action is to talk to your doctor and find out if it’s absolutely necessary that you or your child take their antibiotics, or if it’s reasonable to wait and let your body fight the infection.
If your doctor says it’s okay to wait, you could do something good for your body and as well as for global health. Maybe that same kind of logic ought to be applied to vaccine use as well. Save them only for those who absolutely need them.
Going back to the question in the title of this post, “Is antibiotic resistance a greater threat to public health than COVID?” you could strongly argue the point that, yes, it is. Too bad it doesn’t get nearly the amount of media airtime.

Feel Better Fast. Guaranteed.
Energy+, EDGE, and MentaBiotics make up the Happy Juice supplement stack, with ingredients clinically proven to:
- decrease anxiousness scores by 55%
- decrease irritability scores by 60%
- decrease fatigue by 64%
- decrease anger 54%
- decrease tension by 45%
- decrease confusion by 43%
- decrease overall distress by 49%
- increase good bacteria by 70%
- decrease negative mood by 105%
- increase positive mood by 211%
References
Antibiotic Resistance. https://www.who.int/news-room/fact-sheets/detail/antibiotic-resistance. Accessed 9 May 2022.
Calderón-Parra, Jorge, et al. “Inappropriate Antibiotic Use in the COVID-19 Era: Factors Associated with Inappropriate Prescribing and Secondary Complications. Analysis of the Registry SEMI-COVID.” PLOS ONE, vol. 16, no. 5, May 2021, p. e0251340. PLoS Journals, https://doi.org/10.1371/journal.pone.0251340.
Centers for Disease Control and Prevention (U.S.). Antibiotic Resistance Threats in the United States, 2019. Centers for Disease Control and Prevention (U.S.), Nov. 2019. DOI.org (Crossref), https://doi.org/10.15620/cdc:82532.
Gouin, Katryna A., et al. “Trends in Prescribing of Antibiotics and Drugs Investigated for Coronavirus Disease 2019 (COVID-19) Treatment in US Nursing Home Residents During the COVID-19 Pandemic.” Clinical Infectious Diseases, vol. 74, no. 1, Jan. 2022, pp. 74–82. DOI.org (Crossref), https://doi.org/10.1093/cid/ciab225.
Jan 21, Chris Dall |. News Reporter |. CIDRAP News |. and 2022. “Antimicrobial Resistance Far Deadlier than Thought, Study Finds.” CIDRAP, https://www.cidrap.umn.edu/news-perspective/2022/01/antimicrobial-resistance-far-deadlier-thought-study-finds. Accessed 9 May 2022.
Javed, Faisal. “Truth of Antibiotics That Cause Insomnia.” Business, 8 Oct. 2020, https://ipsnews.net/business/2020/10/08/truth-of-antibiotics-that-cause-insomnia/.
Kisiel, Marta A., et al. “The Risk of Respiratory Tract Infections and Antibiotic Use in a General Population and among People with Asthma.” ERJ Open Research, vol. 7, no. 4, Nov. 2021, pp. 00429–2021. PubMed Central, https://doi.org/10.1183/23120541.00429-2021.
Lai, Chih-Cheng, et al. “Increased Antimicrobial Resistance during the COVID-19 Pandemic.” International Journal of Antimicrobial Agents, vol. 57, no. 4, Apr. 2021, p. 106324. PubMed Central, https://doi.org/10.1016/j.ijantimicag.2021.106324.
Murray, Christopher JL, et al. “Global Burden of Bacterial Antimicrobial Resistance in 2019: A Systematic Analysis.” The Lancet, vol. 399, no. 10325, Feb. 2022, pp. 629–55. www.thelancet.com, https://doi.org/10.1016/S0140-6736(21)02724-0.
Tonazzi, Shera, et al. “Delayed Antibiotic Prescribing to Reduce Antibiotic Use: An Urgent Care Practice Change.” BMJ Open Quality, vol. 11, no. 1, Mar. 2022, p. e001513. PubMed, https://doi.org/10.1136/bmjoq-2021-001513.
“Trends in Antimicrobial Drug Prescribing During the COVID-19 Pandemic.” ASPE, https://aspe.hhs.gov/reports/antimicrobials-during-covid. Accessed 9 May 2022.
Ventola, C. Lee. “The Antibiotic Resistance Crisis.” Pharmacy and Therapeutics, vol. 40, no. 4, Apr. 2015, pp. 277–83.