Listen on: Apple Podcasts | Spotify
Early on in the COVID-19 pandemic, or plandemic, or circus as I like to call it, we saw a distinct difference between how men and women responded to the infection.
Though both men and women (the only scientifically and Biblically supported sexes) saw similar infection rates, men were much more likely to develop severe infections or die from the disease.†
This led some people to believe that estrogen, which is much higher in women, protects you from severe illness, or that testosterone, which is supposed to be much higher in men, makes infections worse.
Many health “experts” vilified testosterone. Listening to them speak, you’d think the best preventative would have been to get on anti-androgen medication. Of course, they were also the ones championing Remdesivir in late-stage COVID-19 patients, which likely killed many people.
A new study shows how ridiculous, and deadly reducing a man’s testosterone might have been, or how much doctors missed the mark by not checking their patients’ testosterone levels.
High Testosterone Protects Men from Severe COVID-19
You’re probably already aware of some of the common risk factors for severe COVID-19. They include:
- Older age
- Male sex
- Obesity
- Diabetes
- Cardiovascular disease
- Systemic inflammation
- Lymphopenia
- Neutrophilia
- Presence of autoantibodies to class-I interferons
Each of these factors plays a role in your susceptibility to severe COVID-19 infection.
But a new study shows that, in men, low testosterone increases your likelihood of a severe infection or mortality. Again, this is specific to men.
According to the study:
- Higher testosterone levels may protect men from COVID-19, based on how testosterone affects immune system function
- COVID-19 infection reduces testosterone levels, and raising testosterone back to usual levels may keep men from developing severe COVID-19 or dying from it
Most men know testosterone as a hormone for building muscle, growing facial hair, and causing an erection. But it does much more, including influencing your immune system.
According to the study’s authors:
we found significant and direct correlations between testosterone levels, lymphocytes, and neutrophils, suggesting a role for testosterone in aberrant immune responses in deceased patients.
Toscano‑Guerra E, at al. Recovery of serum testosterone levels is an accurate predictor of survival from COVID-19 in male patients
The researchers identified a connection between a man’s testosterone levels and his levels of lymphocytes and neutrophils.
There are two types of lymphocytes:
- B cells: They produce antibodies that attack bacteria, viruses, and toxins. If a man’s lymphocytes are low, he won’t be able to produce adequate levels of antibodies to fight a virus like SARS-CoV-2.
- T cells: They destroy the bodies own cells if they’ve already been taken over by viruses or cancer.
Neutrophils block, disable, or digest pathogens like bacteria and viruses.
If a man has low testosterone, and can’t produce adequate neutrophils or lymphocytes, it stands to reason he’d be more likely to get a severe infection, not just COVID-19, but many others.
And yet, nobody is talking about how low testosterone may contribute to a severe COVID-19 infection.
The researchers concluded their paper as follows:
The tight association observed between reinstatement of testosterone and survival from COVID-19 in male patients, along with a reversal of signs of excessive inflammation and immune dysfunction, suggests a potential functional role for testosterone, beyond being a mere biomarker of outcome, in such recovery. Further explorations of mechanistic relationships between testosterone status and SARS-CoV-2 infection outcomes may lead to potential prophylactic or therapeutic interventions to tackle severe and lethal COVID-19 in men.
More simply put, men who got their testosterone levels back up to a healthy level rebounded better from COVID-19, and also experienced a reduction in inflammation and immune dysfunction. They also suggest that future research should look at improving low testosterone levels as a preventative, or testosterone treatment as a therapeutic intervention during infection.
I would add that this study also indicates that a man’s testosterone levels could play a significant role in how he defends himself from many other pathogens beyond SARS-CoV-2.
Read also: Low Testosterone in Men Predicts More Severe COVID-19 Infection
Post-COVID Testosterone Levels
My testosterone levels hovered between 900-1300 ng/dL for four years leading up to getting COVID-19 in April of 2021.
Four months after my infection, I had a comprehensive blood test, and found that my total testosterone had dropped into the 600s. Nothing else about my diet or lifestyle changed during that time.
It wasn’t until about two weeks after my doctor appointment that I wondered if COVID could have contributed. Still, I hadn’t considered how testosterone might influence one’s susceptibility to infection until I read this research paper.
For years, I’ve recommended that men over the age of 30 get their testosterone levels checked each year. About a quarter of men by age 30 already have low testosterone, and the stats get worse with each decade.
In most cases, but not all, lifestyle choices cause low testosterone.
Perhaps this is just another example of how men need to live and eat in a way that maximizes testosterone. Of course, that would mean living counter to today’s culture.
†Even if you take into account the wildly exaggerated COVID deaths and hospitalizations, this sex difference still remains.
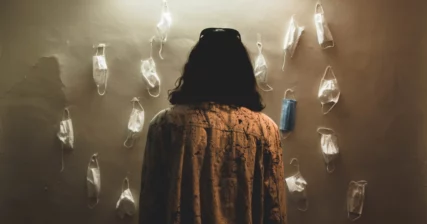
Photo by Amin Moshrefi on Unsplash