Listen on: Apple Podcasts | Spotify
As I explained in my pervious post, I fractured my C6 and C7 vertebrae when I landed head first after going over the handle bars on my mountain bike. The fractures, combined with significant disc degeneration in my C5 and C6 caused compression and flattening of my spinal cord, which then caused Central Cord Syndrome.
The surgeon performed emergency surgery where he and his team removed bone spurs on C5 and C6, removed the remains of my two degenerated discs, replaced them with spacer cages and an artificial bone matrix, and fused my C5 to C6 and C6 to C7 with a two-level anterior cervical fusion and discectomy (ACFD). I also had some bleeding on my brain, but it seems to have been minimal.
Initially, the doctors said it would be a few days before I’d walk and would be in the hospital for a week to a week and a half, and activity for the foreseeable future would be kept to a minimum. Against their recommendations, I demanded to stand up on my own 12 hours after surgery, and later that day said I wanted to walk. The next day, I asked to use the stairs between floors at the hospital and was discharged three days after my surgery.
From the beginning, I also told the medical staff that my hands felt like I’d punched a cement wall. Each staff member told me it was just nerve pain, even though my hands looked like they belonged on the Pillsbury Dough Boy they were so swollen. At a follow-up appointment last week, I told the PA the same thing and she said the same thing: “It’s just nerve pain.” I asked her to order an X-ray on my right hand, which she begrudgingly did. It turns out I was right. My right hand was broken. My left seems to have faired slightly better.
With that as a brief summary, I’ll share what we’re doing to speed up the recovery process, and how that contrasts with the advice I got from the medical team.
I’m sharing this information as a way to detail an “unofficial” case study, not to suggest this for others. If anything, I hope that by sharing the details of what we’re doing in this and future posts, it’ll cause others in similar situations to ask better questions of their medical team. I also hope it causes healthcare practitioners to invest some time into exploring ways their patients can safely recover from similar injuries in less time.
Side Effects of Conventional Guidance Following Spinal Cord Injuries
Following a spinal cord injury and surgery like mine, conventional advice during the first 6-12 weeks includes:
- Wearing a collar (i.e. Aspen collar) at all times. An exception may be to take it off to shower after 2-4 weeks. My PA said I should only do that if I have a shower chair to sit on. I thought that was funny.
- No lifting items over 10 pounds
- Limit exercise to walking or riding on a recumbent bike
Once patients are “allowed” to become more active, the guidance is often akin to lifting soup cans or pink dumbbells.
While I’m all for protecting the area of injury and helping to ensure the fusion heals appropriately, I’m also 100% against allowing the rest of my body to fall apart while that happens. Especially if it isn’t absolutely necessary.
Unfortunately, most patients aren’t led to see things this way. As a result, the average spinal cord injury patient experiences the following:
- 18-46% decrease in muscle cross sectional area in first six weeks, and 45-80% after six months
- significant decrease in ratio of slow twitch to fast twitch muscle fiber type, which reduces fat metabolism, stamina, and endurance
- Up to 126% increase in intramuscular fat within first six weeks and more than a 300% increase after six months
- 3X increased risk of developing diabetes compared to uninjured, comparable adults
- Significant loss in bone mineral density, leading more than 40% of SCI patients to developing osteoporosis or osteopenia, according to one study
These stats are disturbing!
As of 3 1/2 weeks post-op, not a single healthcare professional from my care team has recommended anything related to nutrition, exercise, or lifestyle, other than moderate walking, to combat the metabolic dysfunction associated with spinal cord injury standard of care.
Fortunately, my whole career has centered around diet, exercise, and healthy lifestyle choices. I know I won’t be part of the horrifying statistics above. Unfortunately, most people don’t know.
I hope by documenting my own choices, it’ll generate curiosity in the healthcare professionals that come across my case, and help patients look for better answers for their own recovery.
What I’m Doing For My Recovery
Like my recovery from my distal bicep tendon rupture, we’re using a “shotgun” approach to recovery, throwing anything at it that might work, and that we can afford. There’s plenty more we could do if we had unlimited funds, but I believe what we’re doing is a pretty good start.
I’ll provide a brief summary of each here, and will go into more detail on many of them in future posts.
As a reminder, I’m doing this to:
- Support bone healing in my cervical vertebrae and right hand
- Minimize inflammation
- Maintain as much muscle mass as possible and minimize body fat gain
- Restore strength and function in major muscles and movements as well as restore fine motor skills
- Support nervous tissue regeneration
- Minimize effects of the minor traumatic brain injury (TBI)
Am I certain all of this will work? No. Am I certain any of it will work? No. But I’m pretty sure that most of it will have a positive impact. And I’m absolutely not going to sit around and wait for 20 years for conclusive proof my plan will work, while I wither away into a weak and sick version of my previous self.
High-Protein Diet
A high-protein diet is essential for maintaining muscle mass, supporting better blood sugar regulation and tissue recovery, and crowding out junk food that could negatively affect the healing process.
I started back on my high-protein diet the day after my surgery by eating the highest-protein meals the hospital offered. In addition, I asked my sister-in-law to pick up a case of Isopure and drank two bottles a day of those as well. If you’re part of the nutrition police, I get that Isopure uses artificial sweeteners and colors, but it’s the only whey protein that’s as smooth as water. My throat was extremely swollen from the surgeon moving my esophagus and vagus nerve two inches to the side to access my spinal column. Getting in the extra protein was more important than avoiding the artificial junk.
Though I normally consume 180-200 grams of protein for my 185 pound frame, right now I’m taking in 220-250 grams per day, making up the extra protein by drinking shakes made with whey and collagen, and by eating more cottage cheese and Greek yogurt.
Strength Training Four Days Per Week
Of all of the therapies that could return spinal cord injury patients to normal function and strength, resistance training is surprisingly the least studied. That’s mind-blowing to me since the muscular system and nervous system are so dependent upon one another. I can only assume that research is limited due to concerns about hurting study participants.
At the time of this writing (3 1/2 weeks after injury / surgery) my upper body pressing muscles, forearm flexors and hands are still extremely weak compared to before the accident. Improving pure strength, which is more about training your nervous system to use your muscles than it is about building bigger muscles, requires more frequent, lower volume training.
I currently do four gym-based, full body workouts, and on the off days, do a variety of strength exercises at home.
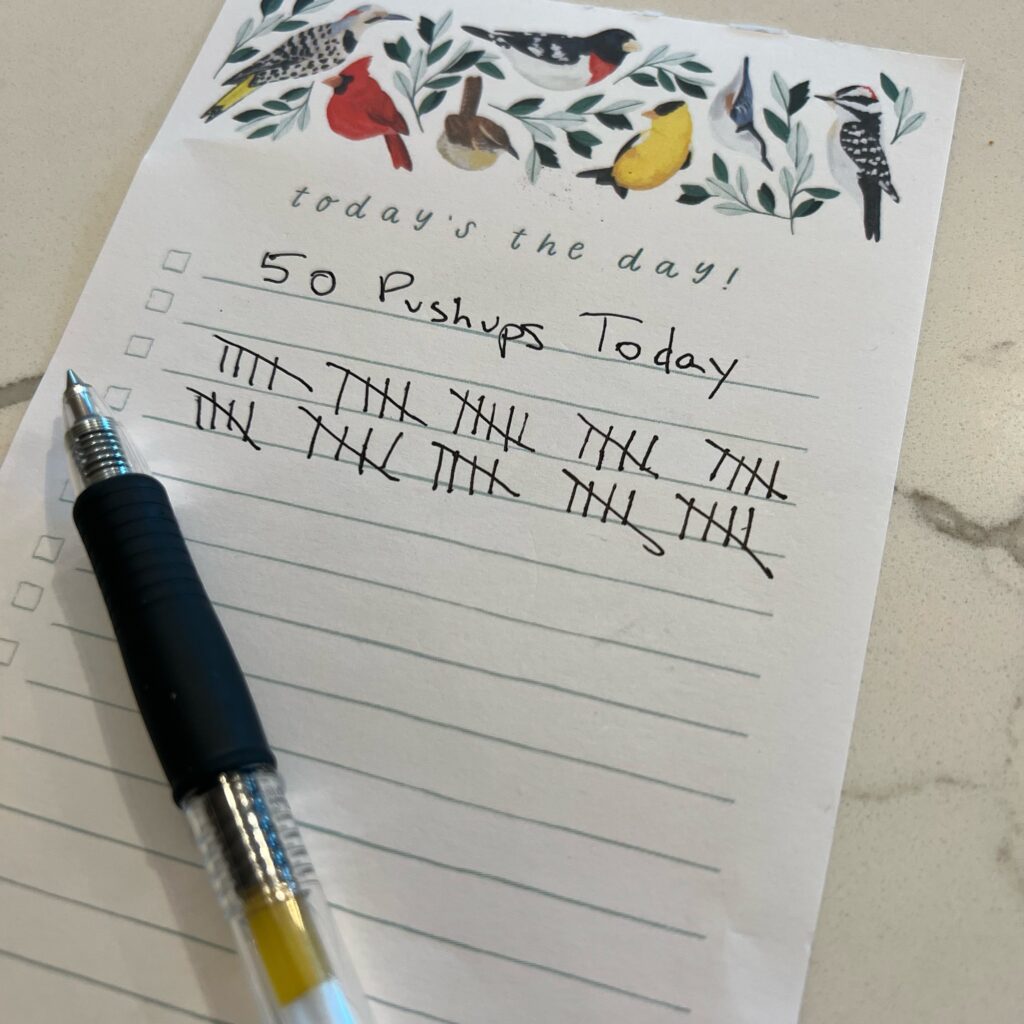
Today, I’m working on completing 50 pushups, which I have to do two at a time, as I don’t yet have the strength to do three.
All that said, I’m not going to sit around and wait for my nervous system function to return to normal before I start using it. I’m going to use whatever I’ve got, and hope that the effort helps me regain my strength and conditioning much faster than a surgeon’s standardized template says it will.
Read also: Why You Should Workout While Injured.
Nutritional Supplements and Other Natural Products
In addition to the Foundational Five and other daily supplements I always take, such as PowerGize, Thyromin, magnesium threonate, and berberine, I’m currently taking:
- N-Acetylcysteine (NAC): Among NAC’s many health benefits, it may support nervous system function by acting as an antioxidant, anti-inflammatory, by reducing neuropathic pain, and by helping to maintain normal mitochondrial function following spinal cord injury
- Curcumin: Research shows curcumin, a compound found in turmeric, may be beneficial following spinal cord injuries. Evidence suggests it may stimulate mobilization of stem cells, act as another potent antioxidant, lower inflammation levels and decrease fibrosis around the injury. Animal research shows it may also help restore motor function and maintain muscle.
- Fortibone®-Containing Collagen: Fortibone® collagen peptides are clinically-proven to increase bone collagen matrix, increasing bone formation. I’m using it to not only support my cervical spine, but also to help heal the broken bone in my hand.
- Melatonin: Though conventional medicine seems decades behind when it comes to supplements, I did get a prescription for melatonin when I was in the hospital and since that’s run out, have continued using the Thorne melatonin I had in the cupboard. Melatonin not only supports restful sleep, it provides additional antioxidant support.* Research shows that maintaining optimal levels is important for bone development and neuroendocrine function.*
- NingXia Greens: This greens blend contains a variety of fruit, vegetable, and botanical extracts and mushrooms, providing additional antioxidants to my diet while also supporting my immune system and digestive tract.* The digestive support is more important than I would have thought, following surgery, from the drugs I’ve needed, and the effects of the spinal cord injury itself.
- Probiotics: I received one dose of antibiotics the day of my surgery, and the other meds have also done a number on my regularity, so I’m taking this probiotic to support a healthy balance of beneficial gut bacteria.*
- Creatine Monohydrate: Unfortunately, I wasn’t using creatine before I landed on my head. Research shows it can reduce spinal cord damage by 36-50%. However, I’m using it now as it helps preserve lean body mass and has been shown to improve strength following spinal cord injury.
- SynaQuell+: SynaQuell+ was specifically formulated for post-impact brain support. I ordered it right after getting home from the hospital. The unique Thorne formula contains:
- Ketones, such as BHB, provide an alternate fuel source for both injured and uninjured brains.*
- BCAAs are important precursors to the neurotransmitters dopamine, serotonin, and norepinephrine.*
- CoQ10 phytosome provides post-impact brain support by reducing oxidative stress and supporting mitochondrial function.*
- DHA, an essential fatty acid found in high concentrations in membranes of the brain’s nerve cells, supports a healthy balance of inflammatory cytokines in the brain.*
- Nicotinamide riboside (NR) promotes NAD+ production, a key substance that protects brain cells.*
- JuvaTone®: JuvaTone supports liver health.* Though this doesn’t necessarily speed up my recovery, I felt it was important to include in my supplement plan after the arsenal of drugs I’d used since the bike accident, including ketamine, fentanyl, Vicodin, oxycodone, dilaudid, gabapentin, maximum strength Tylenol, and my anesthesia. I’m still taking the gabapentin and Tylenol, though I’m slowly weaning off of them.
In addition to the supplements above, Vanessa applies two essential oil-based products to my forearms and hands, which cause a significant, short-term decrease in arm and hand pain.
Biomat
It was immediately apparent after surgery that cold caused pain anywhere on my body other than my head. In fact, I often couldn’t sense “cold,” and would only feel pain in place of a cold sensation. Heat, on the other hand, dulled the pain.
Though my favorite form of heat has been our naked naps, they’re not as easy to fit into our day as a heating pad. Initially, we bought a heating pad from Target, which isn’t the best option with it’s direct heat and EMFs, but it was cheap and quick to get our hands on.
That said, some generous friends sent us a Biomat Mini. It looks like an extra large heating pad, but uses special fabrics and Amethyst stones to heat your body with far infrared rays. The rays penetrate much deeper into the body than a standard heating pad, increasing circulation which may aid in tissue repair and recovery.
Most days, I take a nap on it, lying in a way where the heat reaches my neck and upper back.
I’m brand new to using a Biomat, so I don’t know a ton about it, but from what I have read, it’s pretty impressive. We’re also extremely grateful for getting it as gift.
Peptide Injections
Peptides are becoming increasingly popular as a way to enhance tissue recovery, combat the effects of aging, improve muscle mass, aid in sleep quality, and support optimal sex and metabolic hormones. They’re also seen as a much safer alternative to injecting other hormones. My integrative health doctor prescribed three, which I’m currently using each day: BPC-157, Epithalon, and ARA-290.
Sleep and Naps
I’m well aware of how essential sleep is for recovery. I haven’t been getting a nap in everyday, but I do most days, and we get seven to eight hours of sleep each night.
It didn’t start out that way, though. I thought that I had to sleep on my back when wearing my Aspen collar. After the first week home, I started getting major pain in my upper back. In the middle of one night, I asked Vanessa to do some reading online to find out if I could sleep on my side. She found out that it was okay to do so in the collar, and I’ve been sleeping much better ever since.
Acupuncture
At my two-week follow up appointment with a PA at Regions Neuroscience, I asked her about writing a recommendation for acupuncture. “No, it’s too soon for anything like that,” was her flippant response.
Clearly, she hasn’t kept up on published research for improving spinal cord injury outcomes. For example, consider this statement:
Clinical trials and reviews have suggested that acupuncture effectively manages a range of post-SCI complications, including motor and sensory dysfunction, pain, neurogenic bowel and bladder, pressure ulcers, spasticity, and osteoporosis. The effect of acupuncture on post-SCI orthostatic hypotension and sexual dysfunction remains unclear. Decreased oxidative stress, inhibition of inflammation and neuronal apoptosis, regulation of the expression and activity of endogenous biological mediators, and increased regenerative stem cell production are the possible mechanisms of acupuncture therapy for SCI. Although many limitations have been reported in previous studies, given the evidence for the efficacy of acupuncture, we recommend that physicians should support the use of acupuncture therapy for SCI complications.
Fan Q, et al.
I was hoping that the PA would prescribe acupuncture so our medishare plan could cover it, but I’m getting it done either way. I started the week after surgery. It would seem insane not to get it done based on the scientific evidence supporting it.
Low Level Laser Therapy
I started doing low level laser therapy the same day I started acupuncture. As the authors of a review on low level laser therapy for spinal cord injuries stated:
LLL therapy was able to reduce inflammation and also attenuate neuronal damage after spinal cord damage. The present study illustrates that LLL therapy has positive effects on improving functional recovery and regulating the inflammatory function in the SCI.
Vafaei-Nezhad S, et al.
The lower the level of inflammation around my spinal cord, the faster it can heal and restore normal function.
Other Gadgets, Tools, and Therapies I’m Using to Restore Large and Fine Motor Function
I’m also making time to include a number of other activities and therapies that might improve my fine and gross motor skills. There’s plenty of downtime when riding in the car (since I cannot drive while wearing my Aspen collar) or when sitting down at home. Each of these has a rationale case for expecting it’ll help to return my functions to their old abilities. I do think I’ll end up being a better piano player than I was before, though, as I haven’t played regularly since I was a kid.
- Transcutaneous electrical nerve stimulation (TENS)
- Piano playing and lessons with the Simply Piano app
- Handwriting
- IronPower Gyro hand and forearm strengthener
- Pulling weeds by hand in the lawn
Making the Most of What You’ve Got
I’ve always believed that as human beings, we’ve been blessed with the gift of life. What we do with that gift shows how much we value it.
When I told the medical staff that I wanted to stand up, and then walk the morning after my surgery, it wasn’t an act of defiance or arrogance. I knew that I needed to try. I knew that the sooner I could get myself moving, no matter what pain or uncertainty that might create the sooner I’d be able to move in other ways that would have me recovering faster.
No matter what condition you’re in at this very moment, you have the ability to work toward a condition that’s better than that. To not do so would be to neglect the gift you were given with the life you were blessed with.
Socrates said it another way long ago.
No man has the right to be an amateur in the matter of physical training. It is a shame for a man to grow old without seeing the beauty and strength of which his body is capable.
Socrates
References
AEDG Peptide (Epitalon) Stimulates Gene Expression and Protein Synthesis during Neurogenesis: Possible Epigenetic Mechanism – PMC. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7037223/. Accessed 24 Aug. 2022.
Amorim, Samuel, et al. “Creatine or Vitamin D Supplementation in Individuals with a Spinal Cord Injury Undergoing Resistance Training: A Double-Blinded, Randomized Pilot Trial.” The Journal of Spinal Cord Medicine, vol. 41, no. 4, July 2018, pp. 471–78. PubMed, https://doi.org/10.1080/10790268.2017.1372058.
BPC-157 Health Benefits, Dosage, Safety, Side-Effects, and More | Supplements – Examine. https://examine.com/supplements/bpc-157/. Accessed 24 Aug. 2022.
Dolbow, David. “Exercise Following Spinal Cord Injury: Physiology to Therapy.” Journal of Neurorestoratology, Dec. 2015, p. 133. DOI.org (Crossref), https://doi.org/10.2147/JN.S61828.
Fan, Qianqian, et al. “Spinal Cord Injury: How Could Acupuncture Help?” Journal of Acupuncture and Meridian Studies, vol. 11, no. 4, Aug. 2018, pp. 124–32. PubMed, https://doi.org/10.1016/j.jams.2018.05.002.
FORTIBONE® | GELITA. https://www.gelita.com/en/products/collagen-peptides/fortibone. Accessed 23 Aug. 2022.
GUO, JIAN, et al. “N-Acetylcysteine Treatment Following Spinal Cord Trauma Reduces Neural Tissue Damage and Improves Locomotor Function in Mice.” Molecular Medicine Reports, vol. 12, no. 1, July 2015, pp. 37–44. PubMed Central, https://doi.org/10.3892/mmr.2015.3390.
Gwyer, Daniel, et al. “Gastric Pentadecapeptide Body Protection Compound BPC 157 and Its Role in Accelerating Musculoskeletal Soft Tissue Healing.” Cell and Tissue Research, vol. 377, no. 2, Aug. 2019, pp. 153–59. PubMed, https://doi.org/10.1007/s00441-019-03016-8.
Sanivarapu, Raghavendra, et al. “The Potential of Curcumin in Treatment of Spinal Cord Injury.” Neurology Research International, vol. 2016, 2016, p. 9468193. PubMed Central, https://doi.org/10.1155/2016/9468193.
Stable Gastric Pentadecapeptide BPC 157 and Wound Healing – PMC. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8275860/. Accessed 24 Aug. 2022.
Tardiolo, Giuseppe, et al. “Overview on the Effects of N-Acetylcysteine in Neurodegenerative Diseases.” Molecules (Basel, Switzerland), vol. 23, no. 12, Dec. 2018, p. E3305. PubMed, https://doi.org/10.3390/molecules23123305.
Vafaei-Nezhad, Saeed, et al. “A Review of Low-Level Laser Therapy for Spinal Cord Injury: Challenges And Safety.” Journal of Lasers in Medical Sciences, vol. 11, no. 4, 2020, pp. 363–68. PubMed Central, https://doi.org/10.34172/jlms.2020.59.
Vukojević, Jakša, et al. “Pentadecapeptide BPC 157 and the Central Nervous System.” Neural Regeneration Research, vol. 17, no. 3, Aug. 2021, pp. 482–87. PubMed Central, https://doi.org/10.4103/1673-5374.320969.



