Listen on: Apple Podcasts | Spotify
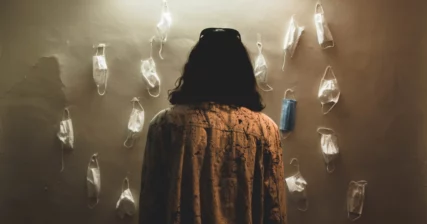
COVID-19 cases have increased significantly in recent weeks. In reaction to the rise in cases, numerous states and cities have rolled back their reopening plans. Masks are mandated across half of the country.
It would be reasonable to assume that the numbers define the count of people who’ve tested positive for SARS-CoV-2 infection. They include more than that count.
It would also be reasonable to assume that the United States counts COVID-19 cases like all other countries do. That isn’t the case either.
The CDC Guidelines for Counting COVID-19 Cases
According to the CDC guidelines, the case and death counts we see as U.S. citizens include both confirmed cases and probable cases. States began adding probable cases to confirmed cases in mid-April, though not all states adopted this more liberal approach to counting right away.
Many other countries count only confirmed cases. Because we use a far more liberal method of counting, it appears that in the United States, COVID-19 is out of control. In reality, it’s a difference in counting methods.
It’s as though in other countries, they’re only counting Dodge Rams, but in the United States, we’re counting all trucks.
Here’s how it works in the U.S. Again, we now count both confirmed cases and probable cases.
A confirmed case meets confirmatory laboratory evidence. You test positive with a standard COVID-19 test. As straightforward as that seems, even the standard PCR test is surrounded by controversy.
A probable case:
- Meets clinical criteria and epidemiologic evidence, but does not include a positive test for COVID-19
- Meets presumptive laboratory evidence and either clinical criteria or epidemiologic evidence, but no positive test for COVID-19
- Meets vital records criteria with no positive test for COVID-19
I’ll share some examples in a moment, but first need to provide the additional CDC definitions.

Feel Better Fast. Guaranteed.
Energy+, EDGE, and MentaBiotics make up the Happy Juice supplement stack, with ingredients clinically proven to:
- decrease anxiousness scores by 55%
- decrease irritability scores by 60%
- decrease fatigue by 64%
- decrease anger 54%
- decrease tension by 45%
- decrease confusion by 43%
- decrease overall distress by 49%
- increase good bacteria by 70%
- decrease negative mood by 105%
- increase positive mood by 211%
Clinical Criteria
The CDC clinical criteria for COVID-19 includes at least one of the following:
- At least two of the following symptoms: fever (measured or subjective), chills, rigors, myalgia, headache, sore throat, new olfactory and taste disorder(s), or
- At least one of the following symptoms: cough, shortness of breath, or difficulty breathing, or
- Severe respiratory illness with at least one of the following:
- Clinical or radiographic evidence of pneumonia, or
- Acute respiratory distress syndrome (ARDS).
And…no alternative, more likely diagnosis.
Laboratory Criteria
Confirmatory laboratory evidence: Standard PCR test.
This is what we’ve known of as COVID tests all along. These should be straightforward enough. And you’d certainly expect them to be accurate. They’re not.
It turns out, a number of initial tests were contaminated. How many? We don’t know.
As a result, some people who were actually negative for the virus, tested positive. Contamination occurred in other countries as well.
Additional studies showed that other tests could lead to a number of false-positive test results, but nobody knows how common this is.
What that means is that some of the people who had COVID or flu-like symptoms, and tested positive for COVID-19, might have just had the flu.
To cloud things even more, some people are testing positive for COVID-19, even after no-showing for their test.
Presumptive laboratory evidence: Antigen or antibody testing that suggests someone could have had COVID-19 in the recent past.
Though it’s logical to think that if you have COVID-19 antibodies, you had and have recovered from COVID-19, that’s not necessarily true. Other coronaviruses can cause you to test positive for SARS-CoV-2 antibodies.
In addition, the tests themselves are far from accurate. So again, using these tests to count COVID-19 case or death numbers can lead to flawed data.
Epidemiologic Linkage
Here’s where things get really questionable. The epidemiological requirements are as follows:
One or more of the following exposures in the 14 days before the onset of symptoms:
- Close contact with a confirmed or probable case of COVID-19 disease (Close contact is defined as being within 6 feet for at least a period of 10 minutes to 30 minutes or more depending upon the exposure. In healthcare settings, this may be defined as exposures of greater than a few minutes or more.), or
- Close contact with a person with:
- clinically compatible illness and
- linkage to a confirmed case of COVID-19
- Travel to a residence in an area with sustained, ongoing community transmission of SARS-CoV-2
- Member of a risk cohort as defined by public health authorities during an outbreak.
Examples of what constitutes a COVID-19 case
Based on the CDC criteria described above, here are some examples of what could be classified as a COVID-19 probable case, and add to the leaderboard plastered all over mainstream media:
- Clinical criteria + Epidemiologic criteria: You have a sore throat and a headache and you went on a date with someone who just found out they’re “COVID-19 probable.”
- Presumptive criteria + Clinical criteria: You test positive for antibodies and have a cough.
- Presumptive criteria + Epidemiologic criteria: You test positive for antibodies and recently visited a loved one in a nursing home, where they’d had an outbreak of COVID-19.
- Clinical criteria + Epidemiologic criteria: Your parent has pneumonia and recently visited another friend who also had pneumonia and was a probable COVID-19 case.
Keep in mind that with the clinical criteria, you’re also supposed to have “no alternative more likely diagnosis.” But when a everything starts looking like COVID-19, what do you think people get told they have?
My father-in-law’s doctor almost listed him with COVID-19, even though he didn’t have it. He had infection in the sac around his heart and tested negative for COVID-19. The doctor wanted him to stay at the hospital on the COVID floor. Had he stayed in the hospital they would have counted him among the hospitalized COVID-19 patients. The hospital could have charged a premium for the room, too.
Here’s the latest case and death counts for the United States.
United States COVID-19 Cases by Day
United States COVID-19 Deaths by Day
Summary
Are the numbers accurate? Based on the CDC guidelines, it would seem that they’re not. Or, more accurately, they don’t articulate the number of people actually infected with COVID-19.
What can we do while we wait for certainty about the severity of the virus and the accuracy of the counts?
The best thing you can do, for this virus or any other, is to get healthy. Lose weight, get blood sugar and blood pressure under control. Eat a healthy, high-protein diet. Follow a good strength training program, and sleep at least seven hours each night.
Follow the CDC guidelines, but remember that your best protection from this, or any other virus, is a strong immune system.

Feel Better Fast. Guaranteed.
Energy+, EDGE, and MentaBiotics make up the Happy Juice supplement stack, with ingredients clinically proven to:
- decrease anxiousness scores by 55%
- decrease irritability scores by 60%
- decrease fatigue by 64%
- decrease anger 54%
- decrease tension by 45%
- decrease confusion by 43%
- decrease overall distress by 49%
- increase good bacteria by 70%
- decrease negative mood by 105%
- increase positive mood by 211%